- 1300 478 375
Menu
The Achilles tendon (or heel cord) is the thick strap that can be felt running down the back of the calf into the heel. When the Achilles tendon pulls on the heel it makes us go up on tiptoe, or pushes us forwards when walking or running. As we get older the tendon becomes less flexible and less able to absorb the repeated stresses of running. Eventually small “degenerative” tears develop in the fibres of the tendon. Sometimes the tendon becomes weakened by the degenerative process to the extent that it tears completely.
With a complete tear, you would probably feel a sudden pain in your heel or calf. Some people say this feels as though someone had kicked them on the calf, or hit them with a squash racquet. Usually the heel becomes painful, swollen and bruised, and it becomes difficult to walk.
The best treatment for a ruptured Achilles tendon is an operation to repair it in most circumstances. This leads to a stronger tendon and a lower re-rupture rate than if treated without an operation.
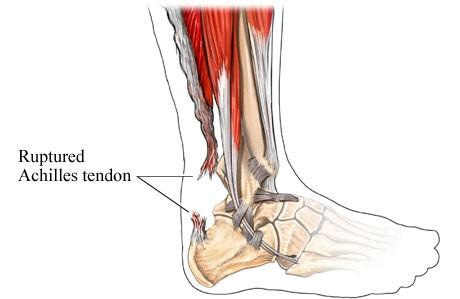
Three small cuts are made over the Achilles tendon. The ruptured ends of the tendon are found and strong sutures are used to stitch the tendon back together. The skin is closed, usually with a dissolving stitch buried under the skin. A plaster is applied to the leg.
Occasionally, there is some delay in making the diagnosis of a ruptured tendon. In this case, the tendon may be scarred in a shortened position. In this situation, a larger incision is used, and more extensive surgery is required, sometimes using another tendon to reinforce or replace the ruptured tendon.
If you are otherwise fit, and there is someone who can collect you afterwards and stay with you overnight, the operation can be done as a day case. This means that you are admitted to hospital, operated on and discharged home on the same day.
If you have other medical problems, or have no-one at home with you, you will have to stay overnight, and you may have to come into hospital the day before for medical tests or treatment. Some people find that they need to stay in hospital the night after surgery because the ankle is painful and they need strong pain killers.
The operation is almost always done under general anaesthetic (asleep). Alternatively, an injection in the back can be done to make the ankle numb while the patient remains awake. The anaesthetist will advise you about the best choice of anaesthetic for you.
In addition, local anaesthetic may be injected into your leg or foot while you are asleep to reduce the pain after the operation even if you go to sleep for the surgery. You will also be given pain-killing tablets as required.
A plaster splint down the back of your ankle and under your foot will be applied while you are asleep.
This is only a half-plaster, to allow for swelling.
You cannot put any weight through your plaster in the first two weeks. You will be provided with crutches when you are discharged from hospital, and a physiotherapist will teach you how to use these.
It is very important that the leg remains elevated most of the time in the first 2 weeks – rest is important. Do not wet or remove the dressings. It is normal to expect:
SWELLING – This can be minimised by elevating your foot above your heart; icing the foot may be helpful
PAIN – You will receive a prescription for pain medication on discharge from hospital. Pain can also be minimised by elevating your leg.
BLEEDING – This always occurs. You may notice some oozing through the bandages.
You will be seen 12-14 days after your operation. A physiotherapist is present. The plaster will be removed and the wound inspected. A specialised ankle brace will be fitted and you will be shown how to adjust it. Continue to rest and elevate your leg as much as possible.
Over the next 6 weeks you will be asked to adjust the brace as follows:
This will be explained and demonstrated to you in detail.
You will be seen again at 8 weeks after the surgery. You will go through another full course of physiotherapy to make your ankle strong and flexible. This will last for several months.
If your ankle is comfortable, you can work in a plaster and sit with your foot up most of the time (basically in a desk job), you could go back to work within a few weeks of surgery. On the other hand, if you do a heavy manual job you may need three or more months off work. How long you are off will depend on where your job fits between these two extremes.
If you have your left foot operated on and have an automatic car you can drive within a few weeks of the operation, when your foot is comfortable enough. Otherwise you will have to wait until the ankle is strong and flexible enough to work the pedals, especially in an emergency situation. This will probably not be for 6-8 weeks after surgery.
When you return to driving you need to take it gradually at first and drive only short distances. Also remember that if you drive before you can stop or manoeuvre in an emergency your insurance will not cover you in the event of an accident.
You can gradually increase your level of activity under the guidance of your physiotherapist. Once you can walk comfortably you can start walking, swimming and cycling, increasing the distance covered gradually. As this recovers you can go back to low-impact, non-contact sports and finally to full contact sports. It is common to take 6-8 months to return to sports such as football or rugby.
You may have moderate pain following the surgery and can take panadeine forte as provided or paracetamol The pain should lessen each day.
You should contact Dr Sterling (through the switchboard of the hospital where you had your surgery), or his secretary on 1300 478 375.
Whilst it is unlikely, if you feel extremely unwell, or there is an unexpected delay in finding Dr Sterling, attend the nearest Hospital Emergency Department.




Take the first step towards your treatment and book your initial appointment with our orthopaedic surgery team.
Prefer the phone? 1300 478 375


