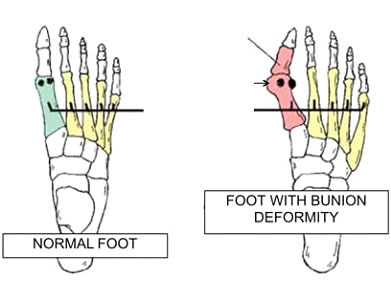
A bunion is a bony prominence over the inner border of the foot at the base of the big toe (hallux) and usually associated with deviation of the big toe (hallux) in an outward direction (hallux valgus). There are several causes. Often there is a family history of bunions (most common). Footwear can also contribute to formation of a bunion. Occasionally a bunion can result from an injury or repetitive stress associated with some sports.
In themselves, bunions do not require surgery. The reason for undertaking an operation is to reduce pain by correcting the deformity. The decision to operate is therefore dependent upon whether the patient experiences painful symptoms and is only undertaken if careful choice of footwear cannot control the symptoms. In other words we do not perform the surgery purely for cosmetic reasons (as the risks of surgery do not justify this).
Details of the minimally invasive surgical technique
Your surgeon will make tiny “keyhole” incisions (approximately 3mm long) through which he will perform the operation. Usually only 5 of these tiny incisions are required. Through these, the tendons and ligaments holding the big toe in the deviated position are carefully released. The surgeon will then use a specialised high speed instrument (a burr) to cut the bones. The surgeon needs to be very experienced in bunion surgery techniques to be able to correctly position and align these cuts. The cuts are made under xray control using a specialised xray machine in theatre. Using various highly specialised instruments the surgeon can make different types of cut and realign the bones involved in the bunion deformity.
The surgeon will also be able to fix the bones in the desired (corrected) position with tiny specialised screws which are also inserted through keyholes using xray guidance. The screws are designed to sit flush to the surface of the bone and so do not cause irritation subsequently.. The actual pattern of cuts and screw fixation is well proven in modern foot surgery techniques (Chevron cut and Akin cut). Thus, the advantages of this minimally invasive surgical technique are that the surgeon is performing establised realignment surgery through tiny “keyholes”. As a result, we expect that the advantages of stable and versatile modern bone cuts will be combined with the advantages of much less invasive surgical technique. Unlike traditional open surgery, no tourniquet is required for this minimally invasive surgery (tourniquet is a tight band placed on the thrigh during surgery to stop the bleeding).
At the end of the operation, stitches are not usually required. The surgeon will inject local anaesthetic around the ankle to make the foot feel comfortable after surgery. The foot is wrapped up in a dressing and bandages. The operation is performed as a daycase surgery.

High speed ‘pencil’ burr use

Specialised “driver” for the burr with controls for the surgeon to control the instruments direction of rotation, speed and torque..

Picture demonstrating the positon of the foot for surgery with the xray machine provideing the surgeons “vision”.
Alternatives to surgery
- To accept your symptoms and try and live with them. Sometimes the bunion becomes worse (they do not get better with time) but this is variable and severity of symptoms also varies from person to person.
- Splints – these may sometimes be helpful in trying to make the foot more comfortable but do NOT correct the deformity and most patients do not find these useful.
- Careful choice of shoes. Most people do not have symptoms from their bunion when barefoot and so choosing a broad enough shoe often helps with controlling/reducing symptoms from a bunion. Custom made shoes can be arranged. Shoes can also be stretched which can be helpful. Choice of shoes or their modification is important to try before considering going ahead with an operation (as it may give sufficient relief to avoid an operation).
General Recovery Facts
- Operation performed under general anaesthetic or regional anaesthetic
- You are able to walk on the heel of the foot the day of the surgery
- You must wear your surgical shoe (heel wedge shoe) at all times
- You may not walk on the foot at all even in the house without this shoe
- You may not drive after the surgery for six weeks unless you have an automatic vehicle and only the left foot has undergone surgery
- The surgical shoe is worn for 6 weeks
Sick Leave
In general 2 weeks off work is required for sedentary employment, 6 weeks for standing or walking work and 6-8 weeks for manual/labour intensive work. We will provide a sick certificate.
Driving
If you have an AUTOMATIC VEHICLE and ONLY LEFT leg surgery then it is likely you will be allowed to drive after your outpatient review at 1 week post surgery. If you have a MANUAL VEHICLE and RIGHT leg surgery then you will NOT be able to drive until 4-6 weeks post surgery (discuss with the surgeon)
*These notes are intended as a guide only and some of the details may vary according to your individual surgery or because of special instructions from your surgeon
POST OPERATIVE COURSE Day 1
- Foot wrapped in bulky bandage and surgical shoe (heel wedge shoe)
- Start walking on the heel in surgical shoe only
- Elevate, take pain medication (usually very little pain)
- Expect numbness in foot 12-24 hours
- Blood drainage through bandage may occur – DO NOT change bandage
- DO NOT remove surgical shoe
Day 7
- Elevate the foot as much as possible and do not remove surgical shoe
- Patients do not usually require any pain medication by this stage
- Keep bandaging dry and do not remove (do not change dressings unless instructed)
- May drive with caution in surgical shoe ONLY if surgery to LEFT foot only and automatic vehicle (otherwise driving at 6-8 weeks post surgery)
10-14 Days
- Follow up in Dr Sterlings rooms for wound review
- Application of toe alignment splint to maintain big toe position
- Alignment splint to be worn inside surgical shoe
- Usually encouraged to begin moving the big toe after 2 weeks post surgery (physiotherapy)
- Shower when incisions healed and dry
6-8 Weeks
- Follow up in the outpatients with an xray on arrival
- Remove surgical shoe If satisfactory xray
- A regular shoe may be worn as comfort allows
- Do not undertake sports or wear high heeled shoes for a further 4 weeks
- Big toe (hallux) alignment splint also to be worn for a further 4 weeks
